Symptoms of Perimenopause: A Complete Guide to the First Signs and What to Expect
Published At
Perimenopause is a stage every woman goes through, yet it’s rarely talked about openly. One day you’re going about your routine and the next you’re wondering: “Why are my periods so irregular? Why am I sweating at night in the middle of winter? Why do I feel so moody lately?”
The truth is, these are very common symptoms of perimenopause—the transition leading up to menopause. While the experience is different for every woman, there are some common signs that help you know what’s going on.
This blog will walk you through the first signs of perimenopause, the typical age of perimenopause, how long it lasts, and most importantly—what you can do to feel better during this time.
What is Perimenopause?
Perimenopause means “around menopause.” It’s the natural transition phase that happens before menopause, when your ovaries gradually begin to produce less estrogen and progesterone. These two hormones play a huge role in regulating your menstrual cycle, mood, energy, and overall well-being. So when their levels start to fluctuate, your body and mind begin to feel the changes.
Unlike menopause, which is officially diagnosed after 12 months without a period, perimenopause isn’t a single moment—it’s more like a journey. Think of it as a rollercoaster ride: your hormones go up and down, periods can become irregular, and your body may send mixed signals that feel unpredictable at times.
This stage can last just a few months for some women, while for others it stretches out over several years. Symptoms also vary widely—some may hardly notice the shift, while others may experience hot flashes, night sweats, mood swings, sleep problems, or changes in skin and metabolism.
In short, perimenopause is your body’s way of preparing for menopause, and every woman experiences it in her own unique way.
When Does Perimenopause Start? (Typical Age of Perimenopause)

Most women begin to notice the first signs of perimenopause in their 40s, though for some, it can start as early as the mid-30s. The exact timing isn’t the same for everyone. It’s influenced by factors like genetics (when your mother or sisters went through it), your lifestyle habits (such as diet, exercise, and smoking), and your overall health.
According to the Cleveland Clinic, perimenopause typically begins about 8 to 10 years before menopause. Since the average age of menopause in women is around 51, that means many women enter perimenopause somewhere between 41 and 43. However, it’s important to remember that “average” doesn’t mean universal. Some women may experience this shift earlier or later, depending on their individual biology and life circumstances.
This wide range in timing explains why women can have very different experiences. While some notice subtle changes, like slightly irregular cycles or mild sleep disturbances, others may encounter more noticeable symptoms such as hot flashes, mood changes, or heavier periods even in their late 30s. Recognizing these early signs helps women understand that what they’re experiencing is a natural transition, not something “wrong” with their bodies.
Fun fact: Some women don’t even realize they’re in perimenopause until their doctor points out the connection between their irregular cycles and other symptoms.
First Signs of Perimenopause

The first signs of perimenopause are often so subtle that many women brush them off as stress, aging, or just “one of those months.” But once you know what to look for, you can start connecting the dots and realizing it’s part of a bigger transition happening in your body.
Irregular Periods
Changes in your menstrual cycle are usually the earliest and most noticeable red flag. Your period might come closer together, get further apart, feel heavier or lighter, or even skip
altogether. These shifts happen because your ovaries aren’t releasing eggs as consistently, and hormone levels start fluctuating.
Example: If you’ve always had a 28-day cycle and suddenly you’re spotting on day 20 one month, skipping your period the next, and then experiencing a very heavy flow—it’s a strong sign that perimenopause has begun.
Hot Flashes and Night Sweats
Few symptoms are as famous—or as disruptive—as hot flashes. They feel like sudden waves of heat that rise through your chest, face, and neck, often followed by sweating, flushing, or even chills once it passes. When these occur at night, they’re called night sweats, and they can leave you tossing, turning, and drenched, making restful sleep almost impossible.
Did you know? Harvard Health reports that up to 75% of women experience hot flashes during perimenopause, making it one of the most common symptoms worldwide.
Sleep Problems
Even without night sweats, hormonal changes can wreak havoc on your sleep-wake cycle. You may find yourself waking up multiple times, struggling to fall asleep in the first place, or feeling groggy no matter how many hours you spend in bed. Over time, poor sleep can lead to fatigue, mood changes, and difficulty concentrating—creating a frustrating cycle that feeds into other symptoms.
Mood Swings and Irritability
If you feel like your emotions are suddenly on a rollercoaster, you’re not alone. Estrogen plays a role in regulating mood, and when its levels fluctuate, you may feel more irritable, anxious, or even depressed. For some, it feels like an intense version of PMS—only more unpredictable. These mood changes are real and hormonally driven, not “all in your head.”
Vaginal Dryness and Changes in Libido
Dropping estrogen levels also affect the vaginal tissues, leading to dryness, thinning, and less elasticity. This can cause discomfort or pain during sex, along with itching or irritation in daily life. Many women also notice a change in libido—sometimes lower, sometimes higher—because hormone shifts, fatigue, and mood changes all influence sexual desire. While not often talked about openly, this is a very real and valid part of perimenopause.
Other Common Symptoms of Perimenopause

Beyond the first signs, you may notice other body changes as perimenopause progresses.
Weight Gain and Slowed Metabolism
Even if you’re eating the same and exercising, you might notice the pounds creeping up—especially around your belly. This is due to hormonal changes slowing down metabolism.
Hair Thinning and Skin Changes
Estrogen supports hair thickness and skin elasticity. With lower levels, hair can feel thinner, and skin may become drier, looser, or more wrinkled.
You can try hydrating products like our Centella Asiatica (Cica) Cream for sensitive, dry skin during this stage.
Breast Tenderness
Similar to PMS, breast soreness and tenderness may come and go unpredictably.
Brain Fog and Memory Issues
Forgetting names, misplacing keys, or struggling to concentrate? You’re not alone. The National Institute on Aging explains that estrogen also impacts brain function, which is why “brain fog” is common.
How Long Does Perimenopause Last?

Perimenopause isn’t a quick phase—it’s a gradual transition that can stretch over several years. On average, it lasts 4 to 8 years, but every woman’s experience is unique. Some women move through it in just a year or two, while others may notice symptoms for nearly a decade.
The length of perimenopause depends on several factors, including genetics, overall health, lifestyle habits, and how your body responds to shifting hormone levels. For example, smoking, stress, and certain medical conditions may lead to an earlier or longer transition.
Perimenopause officially ends once you’ve gone 12 full months without a menstrual period. That milestone marks the beginning of menopause. After this point, your ovaries have stopped releasing eggs, and estrogen and progesterone remain at consistently lower levels.
It’s also common for symptoms to ebb and flow during these years. You may have stretches when things feel stable, followed by sudden flare-ups of hot flashes, mood swings, or irregular cycles. Understanding that this unpredictability is normal can make the journey a little less confusing.
When to See a Doctor

While perimenopause is a natural stage of life, there are times when it’s important to check in with a doctor. Not every symptom you experience during this transition should be dismissed as “just perimenopause.” Some changes may signal other health conditions that need attention.
You should consider seeking medical advice if:
Your periods are extremely heavy or prolonged
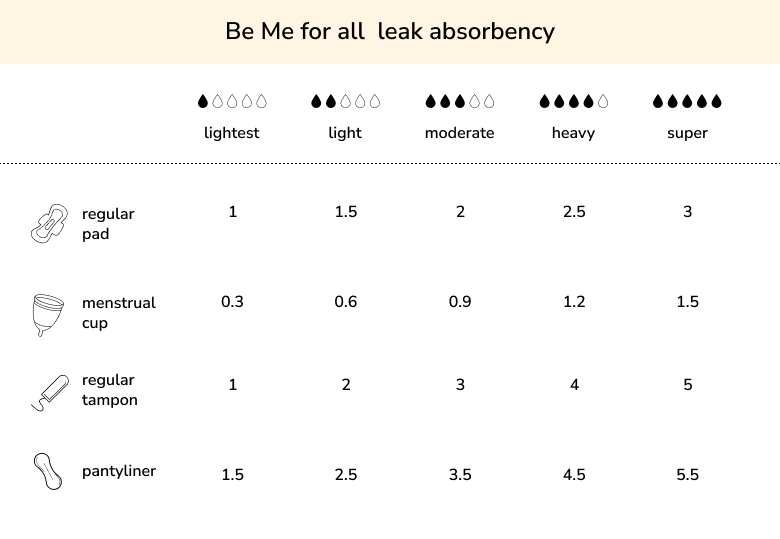
Passing large clots, soaking through pads or tampons every hour, or bleeding for more than a week isn’t typical and could point to issues like fibroids, polyps, or anemia.
You bleed between periods
Spotting after sex or bleeding between cycles may be related to hormone fluctuations, but it can also signal problems with the uterus or cervix that should be ruled out.
Hot flashes or sleep issues interfere with daily life
Occasional discomfort is common, but if night sweats leave you exhausted, or hot flashes are so frequent that they disrupt work, relationships, or your overall quality of life, treatment options are available.
You experience depression or severe mood changes
Feeling sad, anxious, or irritable is common, but if mood swings become overwhelming, or you notice persistent feelings of hopelessness, it’s important to seek support. Mental health changes during perimenopause are real and treatable.
You’re unsure if your symptoms are due to perimenopause or another condition
Thyroid disorders, pregnancy, or other health issues can mimic perimenopausal symptoms. A doctor can help confirm what’s really going on through evaluation and tests.
Remember: listening to your body and seeking help when symptoms feel “off” is not overreacting—it’s taking care of yourself.
Coping with Symptoms of Perimenopause

The good news? While perimenopause can feel overwhelming, there are many ways to manage this transition and ease the discomfort. From simple lifestyle changes to medical support, you can find a balance that works for your body.
Lifestyle and Diet Changes
What you eat and how you live can make a big difference in how your body handles hormonal fluctuations.
Eat a balanced diet
Eat plenty of fruits, vegetables, lean proteins, and whole grains to keep energy levels steady and support overall health.
Cut back on triggers
Avoid triggers like caffeine, alcohol, and spicy foods, which are known to intensify hot flashes and night sweats for many women.
Stay hydrated
Drinking at least 8 glasses of water helps with bloating, skin dryness, and overall circulation.
Prioritize bone health
Keep your bones strong with calcium-rich foods such as dairy, leafy greens, or fortified alternatives, since falling estrogen levels can increase osteoporosis risk.
Exercise and Stress Management
Movement is one of the most effective ways to reduce symptoms, both physically and emotionally.
Regular Activity
Being active on a daily basis helps control weight, improves mood, boosts energy, and supports restful sleep.
Physical Exercise
Try a mix of walking or jogging for heart health, strength training for bones and muscles, and yoga or Pilates for flexibility and balance.
Mind-body Practices
Try mindfulness with practices like meditation, or deep-breathing exercises that calm the nervous system and lower stress, which can ease mood swings and sleep problems.
Natural Remedies and Supplements
Some women find comfort in gentle, natural approaches alongside lifestyle changes.
Chamomile tea
Chamomile tea can soothe the nervous system and promote better sleep.
Spearmint tea
Spearmint tea may support hormonal balance and reduce unwanted symptoms like excess hair growth.
Vitamin D and Omega-3s
Vitamin D and Omega-3s strengthen bones, support brain health, and may improve mood stability.
Always check with your doctor before starting supplements or herbal remedies, since they can interact with medications or may not be suitable for everyone.
Medical Options
If symptoms are more severe or begin to interfere with your daily life, medical treatments can provide effective relief.
Hormone replacement therapy (HRT)
Helps balance declining estrogen and progesterone levels, easing hot flashes, vaginal dryness, and bone loss.
Low-dose antidepressants
Sometimes prescribed to reduce hot flashes and stabilize mood.
Vaginal estrogen creams or rings
Target dryness and discomfort during sex by restoring moisture directly to vaginal tissues.
Sleep aids
May be recommended if insomnia becomes chronic and other approaches don’t help.
Always check with your doctor before starting supplements.
FAQs on Symptoms of Perimenopause
Can perimenopause start at 35?
Yes, early perimenopause can begin in the mid-30s, though most women notice symptoms in their 40s.
What are the very first signs of perimenopause?
Irregular periods, hot flashes, and mood changes are often the earliest symptoms.
Can you still get pregnant during perimenopause?
Yes. Ovulation becomes irregular, but pregnancy is still possible until menopause officially begins.
Does perimenopause cause weight gain?
Hormonal changes can slow metabolism, leading to weight gain, especially around the midsection.
How do I know if it’s perimenopause or just stress?
Since symptoms overlap, tracking your cycles and consulting a doctor is the best way to know.
Living Through Perimenopause With Confidence

Perimenopause can feel like a confusing stage, but it’s also an opportunity to tune into your body and prioritize your health. By recognizing the symptoms of perimenopause, spotting the first signs, and knowing the typical age of perimenopause, you can prepare yourself better for this natural transition.
Remember—you’re not alone. Millions of women go through this stage every year, and with the right support, lifestyle choices, and medical care if needed, you can move through perimenopause with strength and confidence.